Respirator Protection in High-Risk Industries: What You Should Know
From dirty demolition sites, H₂S-contaminated (see here for more) well pads, and bustling ERs, certain professions expose people to air that can damage the lungs in minutes or over years. This article discusses the real work risks that workers encounter and what organizations should do to protect their teams. Also included is a discussion of how modern solutions help compliance and documentation be faster, and easier to manage.
Hazards in Construction
On a renovation site, a masonry crew cuts concrete while a carpenter sands drywall nearby. The air looks clear, but respirable crystalline silica and fine particulates can be high. Without the right controls and a strong respiratory protection program, exposure adds up over time.
• Cutting, demolishing, or grinding masonry products can produce silica dust that can damage lung tissue and produce silicosis, not to mention the potential for other lung disease.
• Even demolition and sweeping floors can liberate a mixture of particulates into the air that include wood, fiberglass, and heavy metals from old paint.
• Confined space atmospheric conditions (crawl spaces / utility vaults) are where it could be vapors of solvents or carbon monoxide from equipment we cannot see but are exposed to.
• Weather changes or wind conditions can lead to plume shifts, making what could have been a “safe” operation hazardous in the middle of the shift.
Oilfield Exposure Risks
Last increased risk exists for workers during a turnaround, as they often move between tank batteries and flare lines and be exposed to H₂S and hydrocarbons vapors and even currently changing oxygen-deficient atmospheres. Before putting on a close-fitting respirator, individuals must have current medical clearance for respirators to confirm that they can safely wear the device. Supervisors also verify that the last fit test for respirator is currently valid and documented, especially if workers are rotating through sites using different models and filters. When working in conditions of increased exposure, a missed clearance or waiting to clearance puts the entire crew at risk.
Healthcare Challenges
Inside an isolation room, a clinician leans over a coughing patient while beeping monitors provide vital signs and doors swing open and close. It is well-known that while utilizing good PPE practices, when completing aerosol-generating procedures, embracing extended durations, or quickly turning over isolation rooms increases exposure. That is why having clear process with time to follow them is important.
• Extended wear can make the seal fatigued or skin irritated, if it is not monitored and rotated depending on the work setting, there is reduced protection change.
• Doffing practices can potentially spread contaminates, utilizing posted practices, buddy checks and/or taking moment to re-review process, can reduce errors.
• Surge staffing ca brings new faces into the environment; utilize online medical evaluations for quick onboarding for float teams without crowding clinics.
Industry-Specific Rules
Employers need a written respiratory protection program that outlines selection, medical evaluations, fit testing, training, and recordkeeping. Employers in Construction Projects are responsible for communicating silica tasks and controls, oilfield and gas operations plan for a specific H₂S and interaction with oxygen; and the healthcare setting plans with isolation protocols and PPE stewardship. Regardless the setting, auditors will be asking for proof of policies matching your training logs and fit testing records to each worker and mask model.
That is where a digital record management is beneficial. A centralized dashboard can track expirations, prompt notifications for the annual fit test, and store documentation by-device. If a foreman or charge nurse just needs to confirm status on-the-go, the system shows which ones are cleared, which respirator model they fit in, and when retraining is due to be completed.
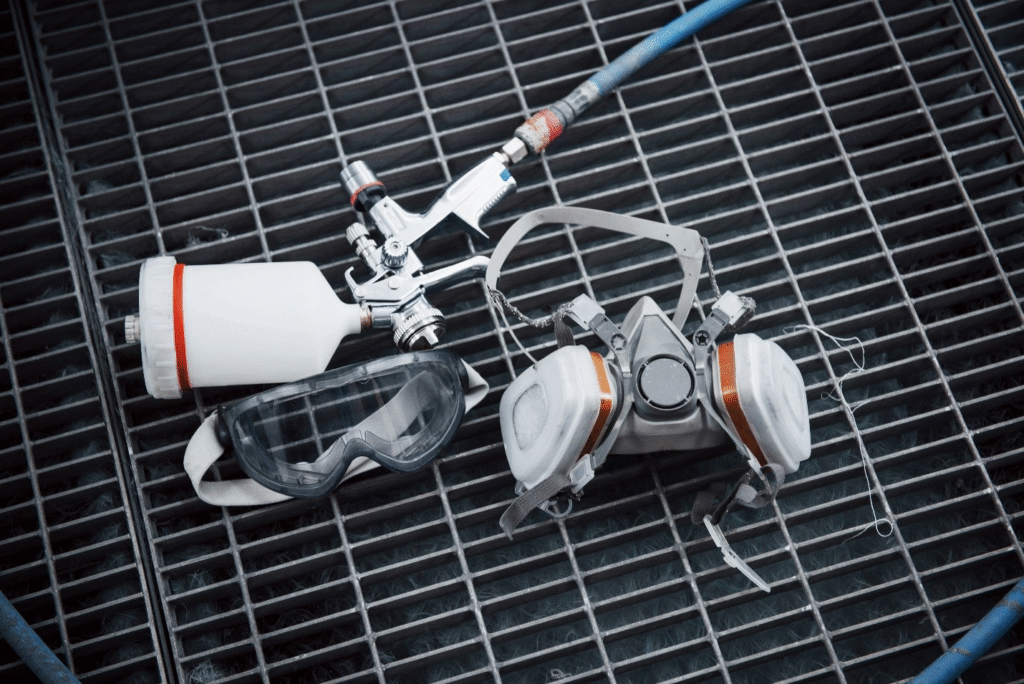
Protective Measures That Work
Every high-risk workplace is well suited with a layered approach; ideally to prevent exposure, then protect followed by altering behavior. Organizations reporting on their leaders who adopt planning and documentation see fewer incidents and quicker and safer shifts.
• Begin with hazard assessments for each task and location; update them as seasons, crews, or materials change.
• Select the appropriate device for the hazard for the worker: filtering facepieces, elastomeric half/full-face, or PAPRs (https://en.wikipedia.org/wiki/Powered_air-purifying_respirator)—all documented in the respiratory protection program.
• Submit online medical evaluations timely and schedule in-person follow-up for flagged evaluations; do not assign a tight-fitting respirator until clearance is obtained.
• Train and practice; train on the same type of respirator in the same environment, and refresh training before anticipated critical outages or during surge periods.
• Use one source to track and manage all fit testing records, training dates, and maintenance logs so supervisors have instant access to verify compliance, even out in the field.
With the appropriate amount of planning, technology and behavior modification, construction, oilfield, and healthcare staffs are able to get used to the shift of breathing easier. With technology reducing the friction of paperwork, the electronic era is allowing the protection of staff, the safety net of sort, while performing Laboratory, oilfield, and healthcare staff with the confidence their focus is getting the job done.